ABOUT BLADDER CANCER
What is bladder cancer?
Bladder cancer is a type of cancer that develops in the lining of the bladder. The bladder is part of the urinary tract, which filters waste products from the blood and produces urine. The urinary tract includes the kidneys, ureters, and urethra. The kidneys filter the blood and produce urine, which is carried to the bladder through the ureters. The bladder stores urine until it is emptied via the urethra.
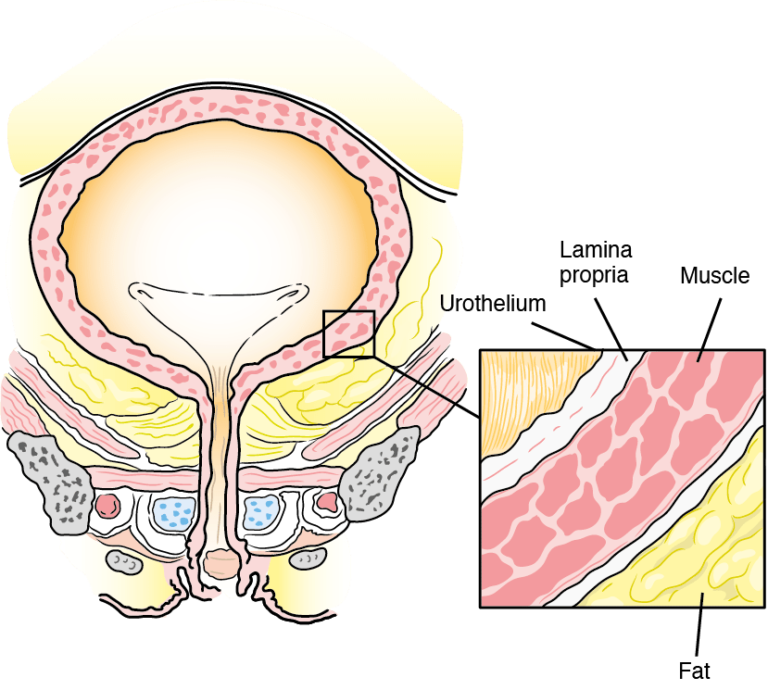 The bladder has four layers:
The bladder has four layers:
- Urothelium – The lines at the bladder that stretches as the bladder fills up; it also prevents the urine being absorbed back into the body
- Laminapropria– A thin layer of connective tissue
- Muscular ispropria– A layer of muscle tissues
- Fatty connective tissue – This separates the bladder from other body organs
What are the symptoms of bladder cancer?
The most common symptom of bladder cancer is blood in the urine without any pain. Other symptoms may include:
- Painful urination
- Urinating very often
- Urinating very suddenly
- Weight loss
- Pain in the back, lower abdomen or bones
- Feeling tired and unwell
What causes bladder cancer?
Several risk factors for developing bladder cancer have been identified. It is important to remember that having a risk factor increases the risk of developingcancer but it does not mean that you will definitely get cancer.
Likewise, not having a risk fact or does not mean that you definitely won’t get cancer.
Factors that may increase risk
- Tobacco smoking
- Exposure to aromatic amines
- Exposure to ionising radiation
- Previous treatment for bladder cancer
- Recurrent or long-lasting urine infections
- Family history of bladder cancer
- Obesity: The most important risk factor for developing bladder cancer is tobacco smoking, which accounts for around 50% of cases. People who smoke have a four- fold greater risk of developing bladder cancer than people who have never smoked. People with the highest risk are those who smoke heavily, started smoking at a young age or have smoked for a long time.
How is bladder cancer diagnosed?
A diagnosis of bladder cancer is based on the results of the following examinations and tests:
Clinical examination
If you have symptoms of bladder cancer, your doctor may carry out a general clinical examination and feel around your abdomen. You are likely to have a urine test to see if your symptoms could be due to a urine infection, and to check for the presence of cancer cells. Your doctor may also perform an internal examination via the rectum or vagina to check if everything feels normal around your bladder.
Cystoscopy
Cytoscopyis a procedure that allows the doctor to see inside your bladder using a light and camera attached to a thin tube that is inserted in to your bladder via the urethra.
You may be awake or asleep during the cystoscopy depending on which type of procedure you have. Flexible cystoscopy uses a soft, bendy tube and is done under local anesthesia, whereas rigid cystoscopy involves a hard, straight tube and is usually done under general anesthesia.
During a cystoscopy, your doctor can take samples (biopsies) of the bladder lining to check for cancer cells.
How will my treatment be determined?
Your treatment will largely depend on the stage of your cancer.
Staging
Staging isused to describe the extent of the cancer overall; this includes its size and position and whether it has spread fromwhere it started. If your cystoscopy shows that you have bladder cancer, you may have a computed tomography (CT) scan and/or magnetic resonance imaging (MRI) scan of your urinary tract. CT is a type of X-ray technique that lets doctors see your internal organs in detail by showing very thin slices of the body. MRI uses magnetic fields and radio waves to produce detailed images of the inside of the body.
The CT and/or MRI scans allow the doctor to assess the location and size of the cancer. You may alsoundergo imaging of your chest, abdomen and pelvis to check for any signs that the cancer has spread.
The results of your biopsies and/or imagingwill confirm what type of bladder cancer you have (urothelialcarcinomaor one of the rare types) and how far your cancer has spread.Your doctor will categorize your diseaseasone of the following:
Palliative care
Palliative care is a term used to describe care interventions in advanced disease, including the management of symptoms as well as support for coping with prognosis, making difficult decisions and preparation for end-of-lifecare. Palliative care in patientswith bladder cancer may include treatment for urinary incontinence, pain and breathlessness.
What are the possible side effects of treatment?
As with any medical treatment, you may experience side effects from your anti-cancer treatment. The most common side effects for each type of treatment are hilighted below, along with some information on how they can be managed. You may experienceside effects other than those discussed here. It is important to talk to your doctor about any potential side effects that are worrying you.
Fatigue is very common in patients undergoing cancer treatment and it can result from the cancer itself or the treatments. Your doctor can provide you with strategies to limit the impact of fatigue, including getting enough sleep, eating healthily and staying active. Loss of appetite and weight loss frequently occur in patients with cancer, and significant weight loss, involving loss of both fat and muscle tissue, can lead to weakness, reduced mobility and loss of independence, as well as anxiety and depression.
Surgery
Most patients recover quickly from TURBT. You may experience blood in your urine and/ora burning sensation when urinating in the first few days after the procedure, but this is normal.
Cystectomy
It is a major operation and it will take some time to recover. You will gradually be able to drink and eat a light diet and you will be encouraged to move around as soon as possible after your operation to speed up your recovery; however, it is normal to feel tired for several weeks after surgery. If you have a stoma you will be taught how to care for it. If you have aneobladder, you will need to learn how to use the muscles in your abdomen to empty your new bladder, as it won’t feel the same as your original bladder.
Radiotherapy
Radiotherapy to the bladder may cause inflammation, which can lead to frequent urination and/or pain during urination. Other common side effects of radiation therapy include fatigue and diarrhea, radiation cystitis.
Chemotherapy
Side effects from chemotherapy vary depending upon the drugs and doses used – you may get some of those listed below but you are very unlikely to get all of them. The main areas of the body affected by chemotherapy are those where new cells are being quickly made and replaced (bone marrow, hair follicles, the digestive system, the lining of your mouth). Some patients find that their sense of taste is affected – changes in enzymes in your mouth can lead to a metallic taste and blisters. Reductions in your levels of neutrophils (a type of white blood cell) can lead to neutropenia, which can make you more susceptible to infections. Most side effects of chemotherapy are temporary and can be controlled with drugs or lifestyle changes.
Long-term side effects
Urination
If you have a urostomy, you will have to learn how to care for your stoma and change your urostomy bags. If you have a neobladder, you will learn how to use your abdominal muscles to empty the new bladder. These changes can be distressing, and it is important to allow yourself time to adjust. Some patients may feel nervous about coping with these changes when going about their normal life, but you will get used to your new urination method. If you tell your family and friends how you feel, they can support you.
Relationships and sex
You may find that your sex life changes after having surgery for bladder cancer. Having astoma can affect the way you feel about yourself and having sex,and your partner might need a bit of time to get used to what your stoma looks like. It’s important for you and your partner to be open about what’s worrying you. In men, the prostate gland is removed during radical cystectomy, meaning you will not be able to ejaculate. If any nerves are damaged during surgery or radiotherapy, you may not be able to get an erection. Your doctor or nurse will be able to help you by prescribing drugs or explaining other options that can help you to get an erection (e.g.penile pumps or implants).
In women, surgery and radio therapy for bladder cancer can narrow or shorten the vagina, making sex painful. Your doctor or nurse will be able to help; for example, dilators can be used to gently and gradually stretch the vagina to make sex more comfortable.
If your ovaries have been removed, you will experience early menopause– your doctor or nurse may suggest hormone replacement therapy to help you cope with this.
What happens next?
Follow-up appointments
After treatment for bladder cancer, your doctor will arrange follow-up appointments to ensure that any recurrences are diagnosed and treated quickly, and long-term side effects are managed effectively. Your doctor will let you know how often you need to return for further follow-up appointments; the schedule will vary between regions. During these appointments, you may have a cystoscopy and/or CT scan.
What if I need more treatment?
Despite the best possible treatment at diagnosis, there is a chance that your cancer may return. Cancer that comes back is called are recurrence. The treatment that you will be offered depends on the extent of the recurrence, your previous treatment and your overall health. Usually, recurrences of bladder cancer are treated in the same way as metastatic bladder cancer, but your doctor will discuss all of the treatment options with you.
Looking after your health
After you have had treatment for bladder cancer, you may feel very tired and emotional. Give your body time to recover and make sure you get enough, but there is no reason to limit activities if you are feeling well. It is important to take good care of yourself and get the support that you need.
- Don’t smoke
- Avoid second-hand smoke
- Exercise regularly
- Avoid weight gain
- Eat a healthy diet as far as possible
- Don’t drink alcohol
- Stay connected with friends, family and other cancer survivors
- Attend regular check-ups
References
- Cancer.Net. 2020.Fatigue. Available from: http://www.cancer.net/navigating-cancer-care/side-effects/fatigue.Accessed 6th June2022.
- ChernyNI; ESMO Guidelines Working Group. ESMO Clinical Practice Guidelines for the management of refractory
- symptoms at the end of life and the use of palliative sedation. AnnOncol 2014; 25(Suppl3): iii143–iii152.
- ClinicalTrials.gov. 2019. Learn about clinical studies. Available from: https://clinicaltrials.gov/ct2/about-studies/ learn. Accessed 6th June 2022.
- Escamilla D Mand Jarrett P.The impact of weight loss on patients with cancer. Nurs Times 2016; 112 (11): 20–22.
- Ferlay J, Ervik M, Lam F, et al. Global cancer observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer 2020. Available from: https://gco.iarc.fr/today. Accessed 1st June 2022.
- Jordan K, Aapro M, Kaasa S, et al. European Society for Medical Oncology (ESMO) position paper on supportive and palliative care. Ann Oncol 2018;29(1):36–43.
- Macmillan. 2018. Side effects of chemotherapy. Available from: https://www.macmillan.org.uk/cancer-information-and-support/treatment/types-of-treatment/chemotherapy/side-effects-of-chemotherapy. Accessed 6th June 2022.
- PaisR, LeeP, CrossS, etal. Bladder care in palliative care in patients: A prospective dual site cohort study. Palliat Med Rep2020;1(1):251–258.
- Powles T, Bellmunt J, Comperat E, et al. Bladder cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol 2022;33(3):244–258.
- Wolin KY, Dart H, Colditz GA. Eight ways to stay healthy after cancer: an evidence-based message. Cancer Causes Control 2013; 24(5): 827–837.